 The influence of the kinetic chain on the patellofemoral can not be underestimated. Because the knee is located mid-way through a weightbearing extremity, it is vulnerable to excessive force from biomechanical faults located both proximally and distally to the knee itself.
The influence of the kinetic chain on the patellofemoral can not be underestimated. Because the knee is located mid-way through a weightbearing extremity, it is vulnerable to excessive force from biomechanical faults located both proximally and distally to the knee itself.
While forces from the foot and ankle have been associated with patellofemoral pain for some time now, the influence of the hip is becoming more of a hot topic as research has demonstrated significant increases in forces and injuries originating from biomechanical faults associated with the hip. A particular pioneer in this research has been Dr. Christopher Powers from the University of Southern California. A Pubmed search on Dr. Powers reveals several significant papers on the topic, specifically one of my favorites from JOSPT on the influence of the kinetic chain on patellofemoral biomechanics.
Examination of the joints proximal and distal to the knee is imperative in the treatment of patellofemoral pain.
I believe a significant reason why “patellofemoral pain” has been such a challenging diagnosis in the past is because we are treating the symptoms, not the cause of the pain, which is many times may be coming from elsewhere within the kinetic chain.
The following is part 7 of the series on solving the patellofemoral mystery:
- Part 1: Introduction – Solving the patellofemoral mystery
- Part 2: What causes patellofemoral pain?
- Part 3: Differential diagnosis of patellofemoral pain
- Part 4: Principles of patellofemoral joint rehabilitation
- Part 5: Specific treatment guidelines for patellofemoral pain
- Part 6: Biomechanics of the patellofemoral joint – clinical implications
- Part 7: Understanding the clinical implications of the kinetic chain: The influence of the hip and foot on the patellofemoral joint
The Influence of the Hip on Patellofemoral Pain
The influence of the hip on the patellofemoral joint has been well documented over the last decade. The biomechanical works of Dr. Powers have shown that excessive hip adduction and internal rotation places the patellofemoral joint in a disadvantageous position.
Unfortunately, our population is dominated by sagittal plane strength and weakness in the coronal and transverse planes. It seems like it is a normal part of daily living now as the majority of our functional tasks take place in the sagittal plane. Even more unfortunate is the fact that exercises outside of the sagittal plane are often neglected in rehabilitation and strength training programs. This creates a significant biomechanical disadvantage.
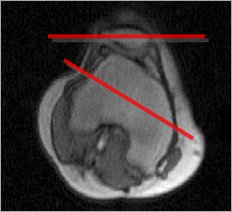
To fully understand the significance of this, imaging the weightbearing knee. When the hip moves into adduction and internal rotation while the foot is planted, the femur will change position around a relatively stable patella (there is movement, just using this as an example). It is the reverse concept that is commonly seen in patellofemoral rehabilitation. The movement, or “tracking” of the patella on the femur is less relevant in this weightbearing position. It is the movement of the femur on the patella that is significant. Below is an example of how the femurs moves on the patella in the weightbearing position, note the patella is fairly stable while the femur rotates internally:

This is likely the mechanism of patellar subluxations and dislocations and the cause of wear and tear of the joint. Patients often describe an injury that occurs when planting and pivoting or planting on an unstable surface. The quadriceps contracts to stabilize the knee while the femur is adducted and internally rotated, resulted in a lateral displacement of the patella in relation to the femur. This can cause an acute injury as well as degeneration over time.
A recent study by Dr. Powers in JOSPT showed that females with patellofemoral pain had greater hip rotation during running, jumping, and stepping down. This also lead to subsequent decrease in hip strength. In fact, another study by Dr. Powers’ group published in AJSM demonstrated that patellofemoral pain in women is the results of decreased hip strength not anatomical variations (wider hips, etc.).

Which brings up a great topic, do you still want to squeeze that ball between your knees and emphasize hip adduction and internal rotation? I would actually recommend just the opposite. I frequently use a piece of Theraband (or even those new knee resistance straps that Theraband just started making) around the patient’s knees during exercise. This will require the patient to isometrically control the hip from adducting and internally rotating while performing mini-squats, wall squats, leg press, and other sagittal plane exercises
The Influence of the Foot and Ankle of Patellofemoral Pain
Just as forces located proximal to the knee can have a significant impact on the patellofemoral joint, forces distal to the knee may also contribute. Treatment for patellofemoral patients should include a thorough assessment of the foot and ankle to establish biomechanical factors that need to be addressed. Orthotic fabrication is often necessary, though off-the-shelf orthotics have had some success in the literature.
Pronation. Excessive pronation of the foot causes a reciprocal internal rotation moment of the tibia. This turn increases the resultant Q-angle at the knee. As we previously discussed in our previous post on the biomechanics of the patellofemoral joint, an increased Q-angle will cause a greater amount of force on a more focal portion of the patella. Furthermore, an internal rotation moment of the tibia also results in internal rotation of the femur and a more laterally displaced patella. This may be a cause of ELPS as discussed previously when we discussed the differential diagnosis of patellofemoral pain.
- Leg Length Discrepancy. I chose to include leg length discrepancy with the group of distal forces as the impact of a longer leg length tends to impact the positioning of the foot and ankle. The longer leg will tend to have a toe-out and pronated position to compensate for the longer length.
- Supination. Patients labeled as “pronators” seem to get all the attention, but excessive supination is likely just as bad. Not only do you diminish the foot’s ability to dissipate force, supination will result in external rotation of the tibia and more force to the patella.
You can see that the position of the foot and ankle when the foot hits the ground is important to evaluate as it will alter the arthrokinematics and patellofemoral joint reaction forces.
It can not be stressed enough that it is imperative that the proximal and distal aspects of the kinetic chain need to be evaluated and treated in patients with patellofemoral pain. I am sure that your outcomes will begin to improve by not neglecting this important aspect of treatment.
Have We Solved the Patellofemoral Mystery?
Probably not, but although the patellofemoral joint may still be a complicated area of sports medicine, I hope that this series has helped take the some of the mystery out of patellofemoral pain! Be sure to go back and review if you missed some of the articles in this series on the patellofemoral joint. In putting the pieces of this series together, remember to:
- Understand the source of patellofemoral pain and realize it might not be from “chondromalacia.”
- Perform a thorough examination and attempt to identify a specific diagnosis, lets stop using the term “patellofemoral pain” and describe the actual diagnosis!
- Consider the basic principles of patellofemoral pain rehabilitation, including understanding the biomechanics of the joint and the biomechanics during exercise.
- Look proximal and distal within the kinetic chain to identify a potential true “source” of patellofemoral pain and stop treating the “symptoms!”
Powers CM (2003). The Influence of Altered Lower-Extremity Kinematics on Patellofemoral Joint Dysfunction: A Theoretical Perspective J Orthop Sports Phys Ther DOI: 14669959
Sign up for my FREE newsletter for even more great content!


 Pronation. Excessive pronation of the foot causes a reciprocal internal rotation moment of the tibia. This turn increases the resultant Q-angle at the knee. As we previously discussed in our previous post on the
Pronation. Excessive pronation of the foot causes a reciprocal internal rotation moment of the tibia. This turn increases the resultant Q-angle at the knee. As we previously discussed in our previous post on the 


